Cooking For A Happy, Healthy Sweet Tooth

MOST OF US find ourselves craving something sweet every once in a while—or perhaps more often than that! Unfortunately, as good as sweet treats taste, they can have a big impact on our dental health.
Sugar And Your Teeth
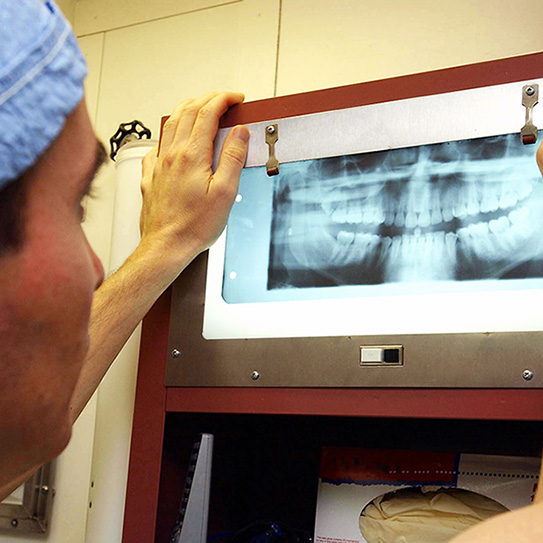
There are many ways that sugar is bad for our overall health, but it’s also specifically bad for our teeth. Our mouths are diverse microbiomes containing dozens of species of bacteria, both harmful and beneficial, that can reproduce multiple times per day. Sugar may taste good to us, but harmful bacteria love it. They eat the sugar that sticks to our teeth and excrete acid that dissolves tooth enamel, leading to tooth decay.
Brushing twice a day and flossing once a day is usually enough to keep the bacteria populations under control, but your teeth will thank your for avoiding excess sugar. So how can we satisfy a sweet tooth craving without also satisfying the cravings of millions of harmful bacteria? By cooking sugar-free desserts, of course!
Healthier Sweet Options
There are a few ways you can cut down on sugar without cutting down on sweets when you’re cooking. Some of them can be pricey, so your budget might play a role in determining which one you use.
Rebaudioside A
Rebaudioside A is a polyol or sugar alcohol produced by Stevia, a leafy South American plant. The FDA has approved rebaudioside A as a safe food additive, which means we can cook with it. But what makes it better for our teeth than sugar? Well, all those hungry bacteria in our mouths can’t digest sugar alcohols. We get to enjoy the sweet taste, but they don’t! The only downside is that it can leave a bitter aftertaste if you use too much. Since you only need one teaspoon to match the sweetness of a whole cup of sugar, it’s easy to overdo it.
Xylitol and Erythritol
Xylitol and erythritol are two more sugar alcohols that serve as excellent sweeteners. You may be familiar with xylitol, because that’s what sweetens sugar-free gum. While it’s even better for your teeth than other sugar alcohols–which is why dentists recommend it–it might not be the best to cook with, as it can cause digestive discomfort if you eat too much of it. Erythritol doesn’t have that drawback, but it can be pretty expensive.
Fruit
Fruit is another great sugar substitute. If you’d rather work with ingredients you already know, unsweetened applesauce, bananas, dates, and figs are four great replacements for table sugar that you can use in many recipes. You’ll end up with desserts that are still sweet and moist, but which contain far less sugar, which your teeth will appreciate. Fruits are sweet because they contain fructose, a type of sugar, but you’ll use less sugar overall by using pureed fruit instead of table sugar.
Need some extra inspiration for a sugar-free treat? Check out this sugar-free cheesecake recipe below!
Keep Up With Your Oral Health Basics
Even if you completely cut out all foods that are bad for your teeth out of your diet, it’s still crucial to maintain good oral hygiene. Brush your teeth twice a day, floss once a day, and come see us for a cleaning appointment every six months! Be sure to bring your favorite sugar-free dessert recipes the next time you come!













My daughter and I love going to see Dr Aparna Sadineni and her professional staff. We never have to wait and the staff knows us like a second family. I highly recommend this office!